Polycystic Ovarian Syndrome (PCOS)
Published by NHC on
Polycystic Ovarian Syndrome (PCOS)
|
Info
|
|
| Description |
A hormonal disorder affecting the ovaries with characteristics of menstrual dysfunction, hyperandrogenism, and polycystic ovaries
|
| Signs & Symptoms |
|
| Causes & Contributors |
|
| Pathophysiology/Aetiology |
|
| Commonly Affected |
|
| Complications |
|
|
Treatment
|
|
| Best Therapeutic Treatment |
Referral for:
Dietary
Consume These:
Avoid These:
Nutrition
Lifestyle
Example Herbal Mix
(May change depending on pathology test results and/or clinical symptoms)
|
| Goals |
|
| Herbal |
Example Herbal Mix
(May change depending on pathology test results and/or clinical symptoms)
|
| Nutritional |
|
| Dietary |
Eat These:
Avoid These:
*Give food swap ideas if necessary
|
| Lifestyle |
|
|
|
|
More
|
|
| Differential Diagnosis |
|
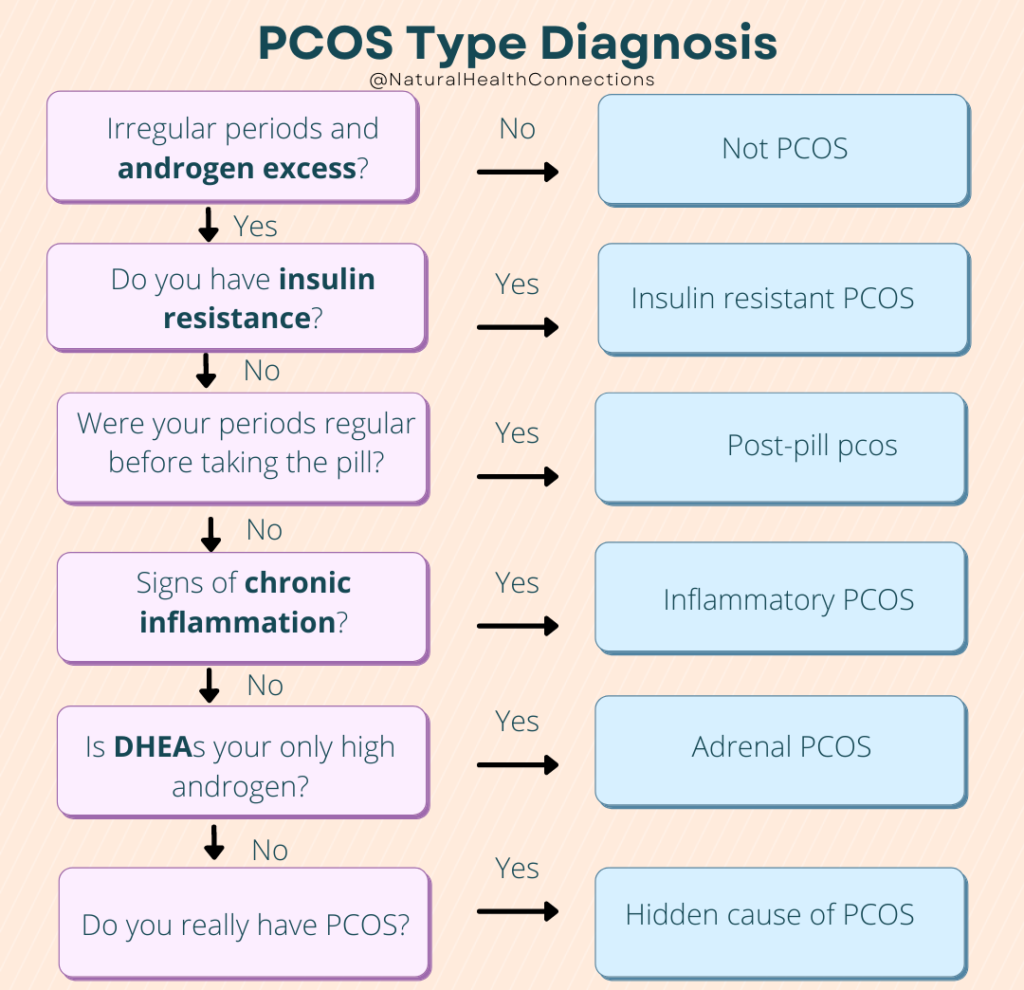
| Diagnostic Criteria |
Rotterdam (2003) Criteria: (2 out of 3 required)
*Exclusion of other aetiologies
|
| Testing/Examinations |
|
| Additional Notes |
|
| Images/Infographics | 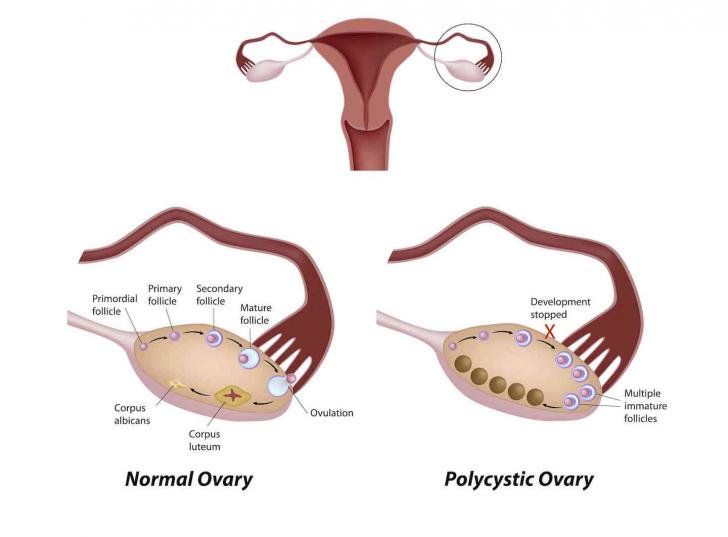 |
Abbott, D. H., Dumesic, D. A., Eisner, J. R., Colman, R. J., & Kemnitz, J. W. (1998). Insights into the development of polycystic ovary syndrome (PCOS) from studies of prenatally androgenized female rhesus monkeys. Trends in endocrinology and metabolism: TEM, 9(2), 62–67. https://doi.org/10.1016/s1043-2760(98)00019-8
Bani Mohammad, M., & Majdi Seghinsara, A. (2017). Polycystic Ovary Syndrome (PCOS), Diagnostic Criteria, and AMH. Asian Pacific journal of cancer prevention : APJCP, 18(1), 17–21. https://doi.org/10.22034/APJCP.2017.18.1.17
Barr, S., Reeves, S., Sharp, K., & Jeanes, Y. M. (2013). An isocaloric low glycemic index diet improves insulin sensitivity in women with polycystic ovary syndrome. Journal of the Academy of Nutrition and Dietetics, 113(11), 1523–1531. https://doi.org/10.1016/j.jand.2013.06.347
Bone, K. (2007). The Ultimate Herbal Compendium. Phytotherapy Press
Braun, L., & Cohen, M. (2015). Herbs and Natural Supplements, Volume 2. Elsevier Health Sciences.
Hechtman, L. (2018). Clinical Naturopathic Medicine. Elsevier Health Sciences.
Hechtman, L. (2018). Clinical Naturopathic Medicine. Elsevier Health Sciences.
Kataoka, J., Tassone, E. C., Misso, M., Joham, A. E., Stener-Victorin, E., Teede, H., & Moran, L. J. (2017). Weight Management Interventions in Women with and without PCOS: A Systematic Review. Nutrients, 9(9), 996. https://doi.org/10.3390/nu9090996
Lee, W. J., Song, K. H., Koh, E. H., Won, J. C., Kim, H. S., Park, H. S., Kim, M. S., Kim, S. W., Lee, K. U., & Park, J. Y. (2005). Alpha-lipoic acid increases insulin sensitivity by activating AMPK in skeletal muscle. Biochemical and biophysical research communications, 332(3), 885–891. https://doi.org/10.1016/j.bbrc.2005.05.035
Marshall, J. C., & Dunaif, A. (2012). Should all women with PCOS be treated for insulin resistance?. Fertility and sterility, 97(1), 18–22. https://doi.org/10.1016/j.fertnstert.2011.11.036
Ndefo, U. A., Eaton, A., & Green, M. R. (2013). Polycystic ovary syndrome: a review of treatment options with a focus on pharmacological approaches. P & T : a peer-reviewed journal for formulary management, 38(6), 336–355.
Sheehan M. T. (2004). Polycystic ovarian syndrome: diagnosis and management. Clinical medicine & research, 2(1), 13–27. https://doi.org/10.3121/cmr.2.1.13
Unfer, V., Facchinetti, F., Orrù, B., Giordani, B., & Nestler, J. (2017). Myo-inositol effects in women with PCOS: a meta-analysis of randomized controlled trials. Endocrine connections, 6(8), 647–658. https://doi.org/10.1530/EC-17-0243
