Premenstrual Syndrome (PMS)
Published by NHC on
Premenstrual Syndrome (PMS)
|
Info
|
|
| Description |
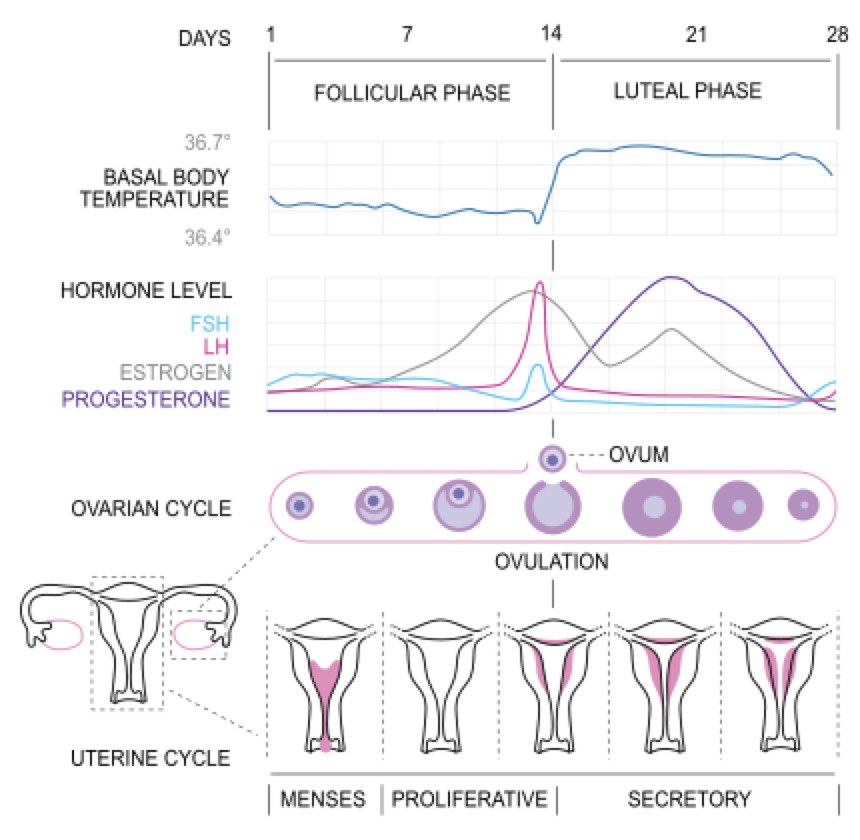
A group of signs and symptoms experienced during the luteal phase of the menstrual cycle which are typically relieved within the first few days of menstruation. PMS symptoms subside by the end of the full flow of menses.
PMDD (Premenstrual Disphoric Disorder)
PMS can be broken down into subtypes/categories:
|
| Signs & Symptoms |
|
| Causes & Contributors |
|
| Pathophysiology/Aetiology |
|
| Commonly Affected | Menstruating women 15-35 years |
| Complications |
|
|
Treatment
|
|
| Best Therapeutic Treatment |
Dietary Advice
Additionally:
Nutritional
Combination Product (use either this or herbal liquid/tablets, not both)
Herbal Treatment
OR
OR
Lifestyle
|
| Herbal |
Combination Product (use either this or herbal liquid, not both)
Example Herbal formula:
Chaste tree 1:2 10ml
St Johns Wort 1:2 20ml
Schisandra 1:2 25ml
Withania 1:1 25ml
Skullcap 1:2 30ml
8ml in water twice a day. Every day of cycle
OR
Chaste tree 1:2 5-40ml a week (Only for two weeks prior to period)
OR
Chaste tree tablets
If fluid retention is present, dandelion leaf 1:1 at 8ml, once a day can be added to the second half of the cycle
|
| Nutritional |
|
| Dietary |
Eat These:
Avoid These:
Increase water intake
*Give food swap ideas if necessary
|
| Lifestyle |
|
| Pharmaceutical |
|
| Combination Products |
|
| Other |
|
|
More
|
|
| Differential Diagnosis |
|
| Diagnostic Criteria |
PMS
PMDD (more sever form of PMS)
|
| Testing/Examinations |
|
| Additional Notes |
|
| Images/Infographics |
|
Bone, K. (2007). The Ultimate Herbal Compendium. Phytotherapy Press
Braun, L., & Cohen, M. (2015). Herbs and Natural Supplements, Volume 2. Elsevier Health Sciences.
Hechtman, L. (2018). Clinical Naturopathic Medicine. Elsevier Health Sciences.
Hechtman, L. (2018). Clinical Naturopathic Medicine. Elsevier Health Sciences.
Henshaw, C. (2007). PMS: Diagnosis, aetiology, assessment and management: Revisiting… Premenstrual syndrome. Advances in Psychiatric Treatment, 13(2), 139-146. doi:10.1192/apt.bp.106.003392
Kwan, I., & Onwude, J. L. (2015). Premenstrual syndrome. BMJ clinical evidence, 2015, 0806.
Noviyanti, N. I., Gusriani, Ruqaiyah, Mappaware, N. A., & Ahmad, M. (2021). The effect of estrogen hormone on premenstrual syndrome (PMS) occurrences in teenage girls at Pesantren Darul Arqam Makassar. Gaceta sanitaria, 35 Suppl 2, S571–S575. https://doi.org/10.1016/j.gaceta.2021.10.103